As always, the opinions expressed here are mine and nobody else’s.
What a wild ride this year has been so far. As my son and I watched the Broncos -Panthers game, it dawned on me that I’ll never hear the famous words from the just retired Peyton Manning anymore. The young next generation QB on the Broncos team though didn’t do too badly though and seemed to keep his cool as he faced the Panthers and end up getting the better of them in the end. Flipping to the wacky Presidential election we’re going through, apparently Vladimir Putin is the new standard of excellence in leadership.
I always look at our nation’s Declaration of Independence and focus on the words “We the people ” in the Constitution therafter, in the 18th century, those were indeed revolutionary words to even think about, let alone write as a declaration.
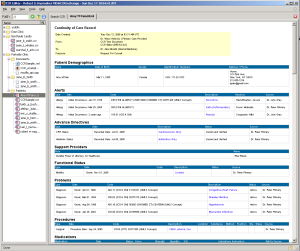
In our world we need to think ever more about empathy and healthcare as never before. Working at Healthcare Providers for some time now, I see the need for a better more efficient and effective way to care for people and believe truly that a combination of collaborative project management, appropriate resource allocation and technology that enhances patient care and safety has the ability to transform patient care in a positive way.
I’ve also seen of late, the return of racist elements I’m society that were previously kept at bay which disappoints me greatly.
Stay focused on the real substance of the world, the care and empathy that we all should have to better understand the human connection that makes us live a more harmonious existence.
If you’re reading this blog post, just look around you and realize all of the good that is in your life and appreciate the ability to be able to give more of yourself for causes such as better patient care through information technology.
Go get ’em!