
It’s been some time since I shared my thoughts as we are well into 2015. ICD-10 for many organizations is well under way and I thought that it might be good to hear from folks other than myself once in a while. So I connected with my good friend and colleague whom I worked with last year, Paul Arel. I had the chance to sit down with Paul and talk about our recently completed engagement working together at a provider organization last year. We discussed his experience with a Computer Assisted Coding (CAC) product that is getting a lot of attention due to the ICD-10 Transition.
Ajay: Thanks for sharing your thoughts on CAC. You’ve been working in other verticals before you got into healthcare IT recently. Tell me the origin of how you started on your recent CAC project?
Paul: My pleasure Ajay. As you’re aware, I have been in the healthcare IT sector for a number of years. When our provider client started its enterprise-wide implementation of a vendor’s CDIS and CAC products to get ready for ICD-10 implementation, they planned on a 3-year project. With about 3 months planned project schedule left, they were having misgivings about the project’s true status and hired me to come in as the new Project Manager. My first task was to get familiar with the project and its players, then ascertain the project’s true delivery status. In so doing, we ended up adding another year onto the project’s delivery schedule.
Ajay: Who were your primary stakeholders and what was their involvement?
Paul: This implementation grew out of the Revenue Cycle side of the hospital. CDIS (Clinical Documentation Improvement System) is utilized by the case reviewers during the patient’s hospital stay. The software helps reviewers make sure that treatment for ailments/injuries follows a path of documented diagnoses. CAC is utilized by the coders to generate billing codes for all care that is given to each patient during their visit or stay. The two work hand in hand to correlate patient care with diagnoses and billing codes, maximizing the revenue stream for the hospital system and driving compliance with the Affordable Care Act. Because of the over-reaching nature of the software and its implementation being enterprise-wide, the stakeholders were numerous and diverse. I would say that the primary stakeholders were the software end users themselves. End user management and the IT support staff were intimately involved in the planning, testing, implementation and monitoring (problem resolution) at every turn during the project. At any one point in time, there were roughly 60 stakeholders intimately involved in the project’s implementation.
Ajay: What was your main challenge especially with the vendor?
Paul: Our main challenge arose as the organization began to realize the gap in knowledge for implementation of the CAC/CDIS products on the scale that the hospital system needed. The chosen software appeared to not be mature at the project’s inception and the disparate EHR systems that the organization used in different markets created a troubling scenario for implementing this software as a standard throughout the organization. At the time, the CAC vendor appeared to have no prior implementation experience on this large and complex an installation, so much of the implementation was learn as you go for everyone involved, including our CAC vendor and the various other vendors.
Ajay: Besides the change in ICD -10 dates by the government, what were the main risks associated with your project go live?
Paul: Risks certainly evolve during a project’s life, but, hands down, the biggest over-riding risk was indeed the interoperability of the software systems involved. While the HL7 standard has been a giant stride forward in interoperability, there still exists much work to be done as the need for pieces of software to communicate as part of a larger whole are constantly expanding. At some point in time, healthcare will require its software vendors to blend their software into a homogeneous system that should appear to the end users to be a single, common interface on the EHR level. At the same time, it needs to allow Operations and Revenue Cycle to pull relevant data from any of the subsystems effortlessly.
Ajay: What issues did you face? Any consistent ones throughout the project?
Paul: Personnel availability was probably the single biggest issue on numerous fronts. Starting with the CAC/CDIS vendor and including most all of the other vendors involved and even within the hospital system itself, personnel availability was the biggest ongoing obstacle to implementation. Most organizations had their personnel “all hands on deck” with the myriad of work needed to test and become ICD-10 compliant in all aspects, as well as performing their regular duties. Congress postponing the ICD-10 implementation date confused and compounded the problem for everybody. And the additional postponement only makes the situation much more problematic for planning in 2015. It is a nightmare right now for all healthcare organizations trying to plan personnel needs for 2015. Nobody knows exactly which personnel will be needed, how many of them will be required, who will be available and, ultimately, if Congress will pull another bonehead move to delay ICD-10 implementation yet again.
Ajay: Bonehead indeed! Healthcare Provider organizations have spent billions to date and hopefully the ecosystem realizes that. Ultimately it’s you and I and the patient population of the United States that pays for all of that.
Ajay: Did you have any outside training organizations train the coders?
Paul: End user training was conducted by the CAC/CDIS vendor, as part of their contract with the organization for implementing their software. Additional training was conducted by Revenue Cycle staff and additional training is also available as part of the vendor’s ongoing usage contract.
Ajay: How was the implementation of the software left, in the wake of the ICD-10 delay?
Paul: The software is designed, like many of its kind, to be compliant for both ICD-9 and ICD-10 usage. When the project ended, the provider organization was utilizing the software in ICD-9 mode only. Provisions were underway to continue with ICD-10 training and the roll-out of dual coding (ICD-9 and ICD-10 coding simultaneously) to help familiarize end users with ICD-10 coding before the nation transitions.
Through another project, we tested ICD-10 functionality, but, as with most hospital systems, a thorough end-to end, integrated test of ICD-10 is still necessary. Hospital systems not only need to be certain that ICD-10 codes pass through their software systems, but that the reimbursements they receive are truly being maximized under the new ICD-10 system. There needs to be validation on two fronts: 1) that the care each patient receives benefits their well-being in the most efficient manner, and 2) that the patient stay generates the maximum return on the dollar for the hospital system. Combined together, these two aspects will drive the hospital system towards providing the best possible care for all patients today and in the future. Despite the politics behind the Affordable Care Act and how/when it is implemented, I feel that this is the underlying goal of both healthcare providers and the government.
Ajay: Thanks for your time Paul. All the best for 2015 and beyond.
Paul: Thanks Ajay. Same to you.
About Paul Arel:

About Paul:
Paul Arel, PMP, MCSE, is a Senior Information Technology Project Manager with over 10 years of experience in project management, having spent much of his career providing services in the healthcare sector. Paul graduated from Miami University (Oxford, Ohio), started his professional career as a Practice Administrator for Art of Smiles Dentistry for more than ten years. During his tenure there, he became a certified EHR trainer for Dentrix, and the practice became a test site for the vendor, providing continual feedback for enhancements and software improvements. Paul guided the practice towards the cutting edge of technological innovations in the field, being one of the first practices nationwide to implement digital x-rays, voice-activated charting & integrated intra-oral photography. He then moved into IT full-time, and earned his Microsoft Certified Systems Engineer (MCSE) certification. He continued to refine his path in IT and healthcare, becoming a Project Manager. Though his projects took him into many fields, including construction, IT infrastructure and automotive support, he continues to be passionate for healthcare. As he was assisting ever-larger healthcare organizations with their project management initiatives, he also earned his Project Management Professional (PMP) certification. His experience led to managing projects for Cincinnati Children’s Hospital and numerous physician practices. Most recently, his healthcare IT expertise was brought to bear when he was hired to manage an enterprise-wide installation of 3M’s CAC/CDIS products for Mercy Health (formerly Catholic Health Partners).
 All of us have been to the ER for either our own ailments or those of our families. I read an article here that details some of the unfortunate experiences of some people who seemed to have received the raw end of the stick. This is the article posted today, May 1st, 2018. It’s worth the read. Think about your own Emergency Room experiences. How do we get better over time? How frequent is this experience?
All of us have been to the ER for either our own ailments or those of our families. I read an article here that details some of the unfortunate experiences of some people who seemed to have received the raw end of the stick. This is the article posted today, May 1st, 2018. It’s worth the read. Think about your own Emergency Room experiences. How do we get better over time? How frequent is this experience?
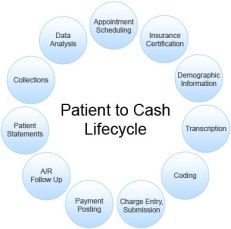 Having worked with Revenue Cycle professionals over the last few years, gives me a finer appreciation of the work that provider organizations have to do to get paid. We’ve all received those bills we thought that the insurance company would have taken care of and wondered why are we receiving this? Why can’t I get through to the company that has sent me this? Did I really get disconnected after holding on this phone for 15 minutes? Frustration can certainly mount. I know it does for my family when trying to figure out next steps. According to an article from Healthcare Finance that I recently read, the top 5 medical claim denials that are the most common are:
Having worked with Revenue Cycle professionals over the last few years, gives me a finer appreciation of the work that provider organizations have to do to get paid. We’ve all received those bills we thought that the insurance company would have taken care of and wondered why are we receiving this? Why can’t I get through to the company that has sent me this? Did I really get disconnected after holding on this phone for 15 minutes? Frustration can certainly mount. I know it does for my family when trying to figure out next steps. According to an article from Healthcare Finance that I recently read, the top 5 medical claim denials that are the most common are: I know many folks are eagerly looking forward to next week in Vegas and
I know many folks are eagerly looking forward to next week in Vegas and 



